Column We Read For You All the Studies on the Florence Method, Which is Currently Taking the World by Storm
The Florence method is an advanced treatment for spinal canal stenosis that has been introduced mainly in Europe and South America.
Medical facilities around the world have published research results regarding the Florence Method treatment.
This time, we would like to introduce papers related to the Florence method.
What is the Florence Method?
The Florence Method is a Low-Risk, minimally invasive treatment for spinal canal stenosis.
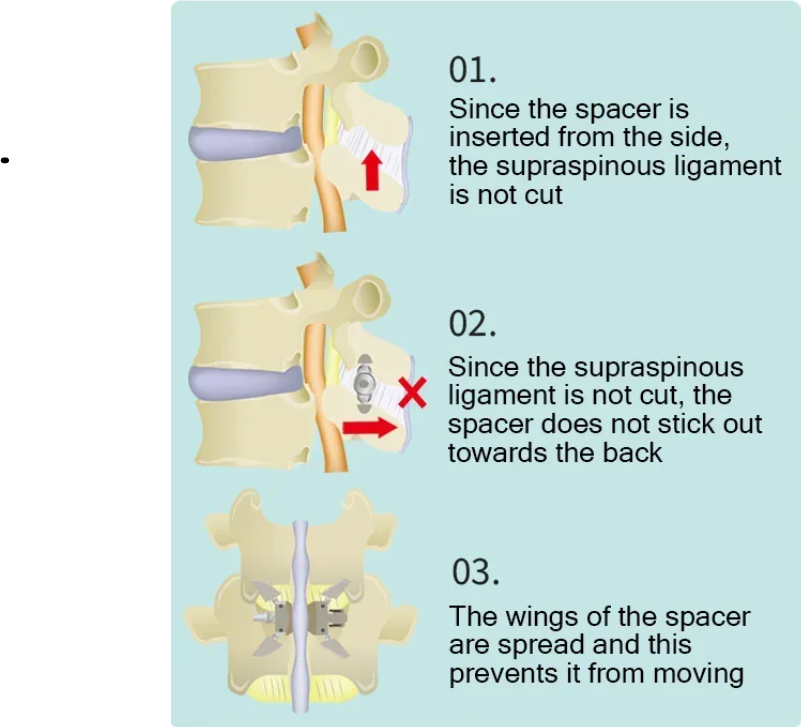
A spacer is inserted percutaneously under local anesthesia and sedation to widen the narrowed spinal canal. It can be removed after treatment.
By inserting a Lobster spacer, it is possible to stabilize the vertebral body while maintaining spinal rotation and flexion, widening the spinal canal, suppressing disc protrusion, and reducing ligamentum flavum thickening. Symptoms such as pain and numbness are resolved by widening the narrowed spinal canal.
Papers on the Florence Method
Medical facilities around the world have published research results regarding Florence Method treatment.
It should be noted that the paper has been published in Europe and elsewhere, and the treatment names in the paper are “Lobster” and “Lobster Project,” which are well-established in Europe and the Americas.
Here we will explain the Florence method introduced in the following three papers.
1. Luigi Manfre, et al. Successful use of percutaneous interspinous spacers and adjunctive spinoplasty in a 9 year cohort of patients. Journal of NeuroInterventional Surgery. 12(7), 2020.
2. Luca Jacopo Pavan, et al. Clinical and radiological outcomes following insertion of a novel removable percutaneous interspinous process spacer: an initial experience. Spinal Neuroradiology. 64(9), 2022.
3. Stefano Marcia, et al. Feasibility, safety, and efficacy of a new percutaneous interspinous device: a retrospective multicenter study. Neuroradiology. 2024.
Regarding adaptation of the Florence method
The Florence method is applicable in the following cases:
 Schizas grade C to D spinal stenosis or grade B spinal stenosis that has not responded to conservative treatment (Manfre 2020)
Schizas grade C to D spinal stenosis or grade B spinal stenosis that has not responded to conservative treatment (Manfre 2020)
 Lumbar spinal canal stenosis that was ineffective after 3 months of conservative treatment (Pavan 2022)
Lumbar spinal canal stenosis that was ineffective after 3 months of conservative treatment (Pavan 2022)
 Neurogenic intermittent claudication due to lumbar spinal stenosis or foraminal stenosis (Marcia 2024)
Neurogenic intermittent claudication due to lumbar spinal stenosis or foraminal stenosis (Marcia 2024)
What is the Schizas classification of spinal canal stenosis?
The Schizas classification is a classification of the severity of spinal canal stenosis defined by Dr. Schizas of Switzerland.
Grade A: Spinal fluid is found within the dural sac, but its distribution is uneven.
Grade B: rootlets occupy the entire dural sac, but spinal fluid is still visible
Grade C: No rootlets are observed, the dural sac is a uniform gray signal, and no spinal fluid signal is observed. Epidural fat is seen posteriorly.
Grade D: No rootlets and no epidural fat posteriorly.
Grade A is defined as no or mild stenosis, grade B as moderate stenosis, grade C as severe, and grade D as severe stenosis. *1
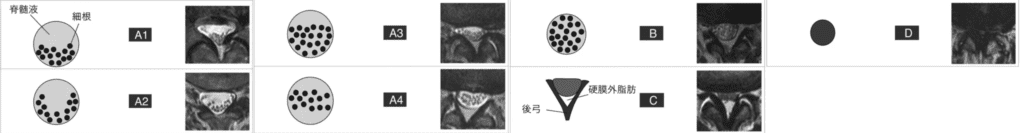
*1 Reference source: Schizas C, et al. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine, 2010, 35.
Looking at this classification, the paper states that the Florence method is suitable for moderate to severe spinal canal stenosis.
About the therapeutic effects of the Florence method
Dr. Manfre’s research
A total of 688 patients were treated, 256 with percutaneous interspinous device alone and 432 with concurrent spinal augmentation of the adjacent spinous processes.
After insertion of the Lobster spacer, enlargement of the spinal canal and intervertebral foramen and improvement in thickening of the ligamentum flavum were observed. Symptoms decreased from 3.2 to 1.3 on the Zurich Claudication Questionnaire score after 3 months of treatment, a significant improvement, and remained the same at follow-up 12 months after treatment.
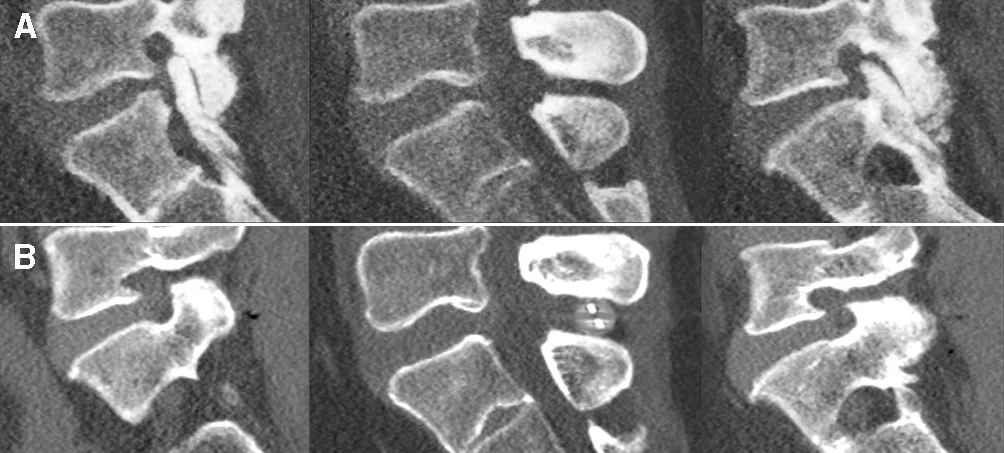
(A) CT image before treatment showing lumbar spinal stenosis. (B) After inserting the interspinous spacer, the spacing between spinous processes and the spinal canal can be enlarged.
There were no immediate complications and no patients required epidural injections or nerve blocks after treatment.
Dr. Pavan’s research
Forty-nine patients were treated and follow-up was available for 48. There were no reports of complications after the treatment.
A follow-up three months after treatment showed a significant reduction in symptoms, and the average area of the intervertebral foramina increased after treatment.
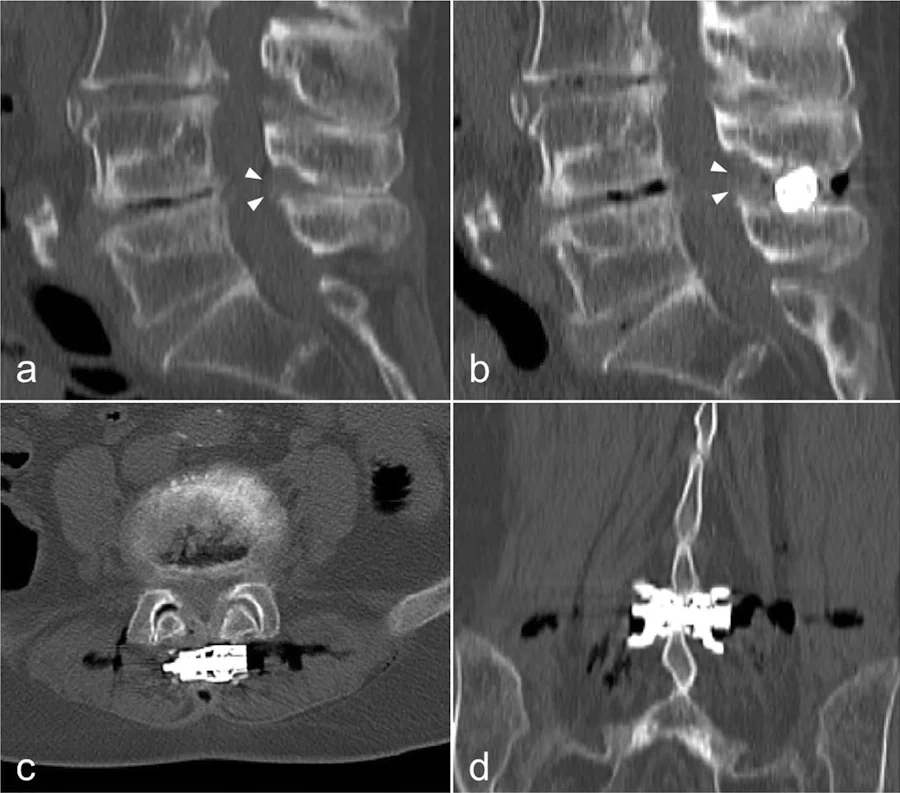
a: CT image showing spinal canal stenosis due to disc protrusion at L4/5 and thickening of the ligamentum flavum. b-d: Post-treatment CT images showing enlargement of the spinous process interval and reduction of ligamentum flavum thickening
Dr. Marcia’s research
258 patients were treated. A follow-up after 6 months of treatment showed improvement in symptoms in 99.6% of patients.
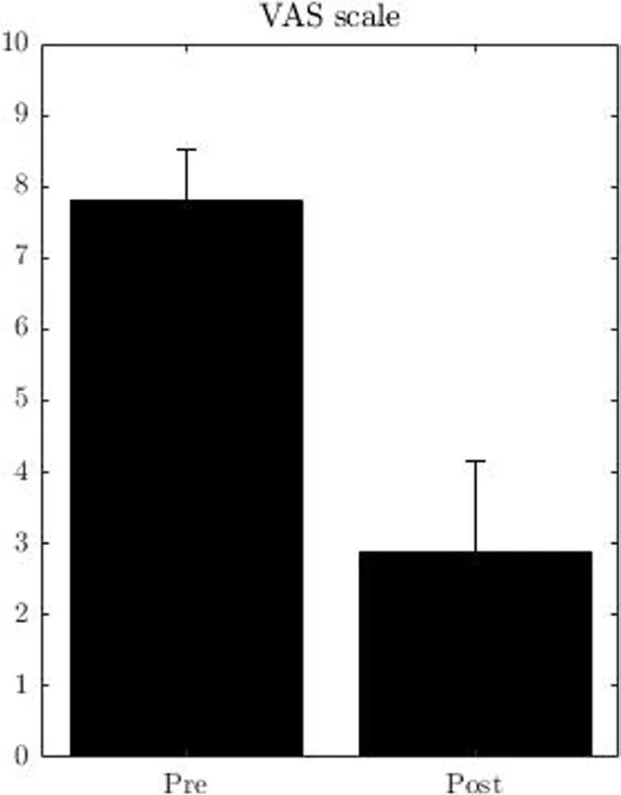
Improvement in Pain
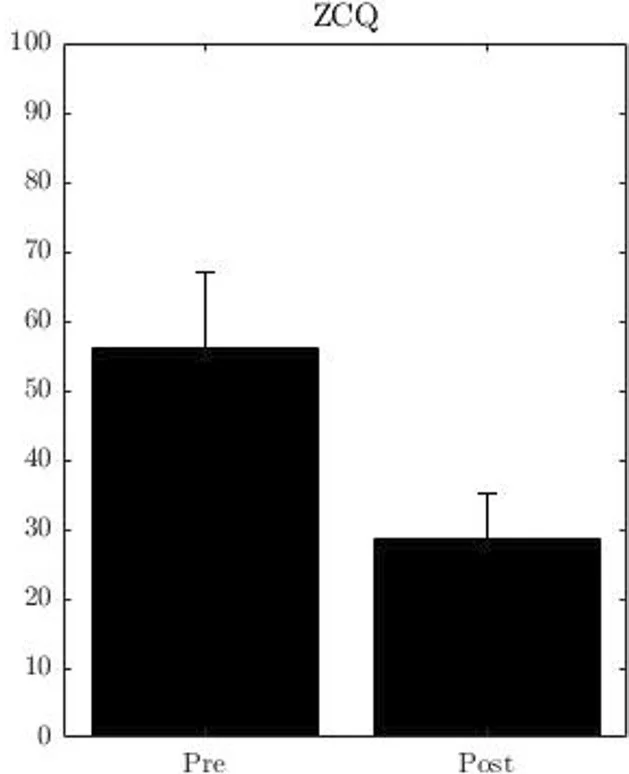
Improvement of intermittent claudication
In both papers, treatment using Lobster spacers is considered to be an effective, safe, and minimally invasive treatment.
If you have been diagnosed with spinal canal stenosis and are suffering from lower back pain or intermittent claudication, please consider seeing us at our clinic.