Column What is the Age Limit to be Eligible for Spinal Stenosis Surgery? Can You Still Get it Even if You are at an Advanced Age?
October 25, 2024
Spinal stenosis is a condition in which the spinal canal (the space in the spine that contains the spinal cord and spinal nerves) becomes progressively narrower. According to a survey report on spinal surgery by the Japanese Society for Spine Surgery and Related Research, it is the most common spinal disorder in Japan (*1).
(*1) : Hiroshi Nohara et al. “Japanese Society for Spine Surgery and Related Research Spinal Surgery Survey Report”, “Japanese Journal of Spine Surgery and Related Research”, Vol. 15, No. 2, 2004.
When the spinal canal narrows, the nerves passing through it are compressed, causing pain and numbness from the lower back to the legs. Intermittent claudication, in which pain and numbness occur in the buttocks and legs when walking and ease up when resting, is a characteristic symptom of spinal canal stenosis.
The stronger the symptoms, the more likely surgery will be considered, but in this article we will be focusing on the age at which each type of surgery can be performed.
Surgical Treatment for Spinal Canal Stenosis
The most common surgical treatments for spinal stenosis are lumbar laminectomy and spinal fusion.
Lumbar laminectomy
This is a procedure that is performed under endoscopy. Under general anesthesia, an 18 to 20mm incision is made in the skin on the back, and an endoscope tube is passed through the incision. The procedure involves removing part of the lamina and the thickened ligamentum flavum to relieve pressure on the nerves and widen the spinal canal.
The hospital stay takes about a week.
If you also have spondylolisthesis or spinal stenosis, you may need to receive fusion surgery after the decompression surgery.
Spinal fusion surgery
This is a surgery to stabilize the spine performed under endoscopy and an X-ray fluoroscopy device. Under general anesthesia, the skin on the back is cut open, the degenerated intervertebral disc is removed, and a man-made device called a cage which is filled with bone taken from the hipbone is inserted to reshape the spine. After that, the vertebrae are held in place with screws and rods.
This type of surgery is indicated in cases of lumbar spondylolisthesis or lumbar instability.
The hospital stay is relatively long, lasting 1 to 2 weeks.
The age limits for surgical treatment
On paper, there is no reason why you cannot receive surgery just based on your age.
As a matter of fact, spinal stenosis is the most common disease among the elderly. Research shows that the prevalence of spinal stenosis is between 90 to 100% among people aged 60 and over, and 80% among those aged 70 (*2). And, surgical operations are also often performed on elderly patients (*3).
*2: Khalepa R.V., Klimov V.S., Rzaev J.A., Vasilenko I.I., Konev E.V., Amelina E.V. SURGICAL TREATMENT OF ELDERLY AND SENILE PATIENTS WITH DEGENERATIVE CENTRAL LUMBAR SPINAL STENOSIS. Russian Journal of Spine Surgery (Khirurgiya Pozvonochnika). 2018;15(3).
*3 : Deyo, R. A., Hickam, D., Duckart, J. P., Piedra, M. Complications After Surgery for Lumbar Stenosis in a Veteran Population. Spine. 2013;38(19).
Post-operative complications
Even if there is theoretically no age limit for surgical treatment, there still is one important point to keep in mind.
The incidence of comorbidities is high in elderly patients, and is estimated to be between 60 and 73.9%. Comorbidities are said to increase the incidence of postoperative complications and make the recovery period longer (*4).
Diabetes, dyspnea, chronic obstructive pulmonary disease, and the use of steroids in conjunction with chronic diseases increase the risk of postoperative complications (*5).
In addition, research has shown that previous surgical history, hospitalization for conditions other than lumbar disease, and the type of surgery performed can also affect the risk of postoperative complications (*6).
The “fatal complications” listed in the table below refer to cardiopulmonary arrest, acute myocardial infarction, respiratory failure, pulmonary embolism, bacterial pneumonia, aspiration pneumonia, pneumonia of unknown cause, and strokes, while surgical wound complications refer to bleeding, hematoma, seroma, non-healing surgical wounds, and infection.
| Fatal complications | Surgical wound complications | |
|---|---|---|
| Previous surgeries | ||
| ・None | 3.0% | 1.0% |
| ・Yes | 4.0% | 4.6% |
| History of hospitalization for conditions other than lumbar disease | ||
| ・None | 2.8% | 1.2% |
| ・Yes | 3.4~5.0% | 1.3~2.4% |
| Type of surgery performed | ||
| ・Excision | 2.1% | 0.9% |
| ・Fusion (1 to 2 locations) | 4.7% | 1.6% |
| ・Fusion (anterior and posterior at the same time, 2 or more locations) | 5.2% | 2.2% |
(Richard A. Deyo, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults より)
*4: Khalepa R.V., Klimov V.S. Lumbar spinal stenosis in elderly and senile patients: problem state and features of surgical treatment. Russian journal of neurosurgery. 2017;(1).
*5: Deyo, R. A., Hickam, D., Duckart, J. P., Piedra, M. Complications After Surgery for Lumbar Stenosis in a Veteran Population. Spine. 2013;38(19).
*6: Richard A. Deyo, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303(13).
Older patients often have comorbidities, and the physical strain of surgeries such as resections and fusions performed under general anesthesia can increase the risk of postoperative complications and delay recovery.
Treatments at our clinic
Our clinic performs the Florence and Cellgel Methods on spinal stenosis.
Both of these procedures are minimally invasive and have a low impact on the body. We recommend them to patients who wish to avoid surgical procedures such as spinal fusion, which require general anesthesia.
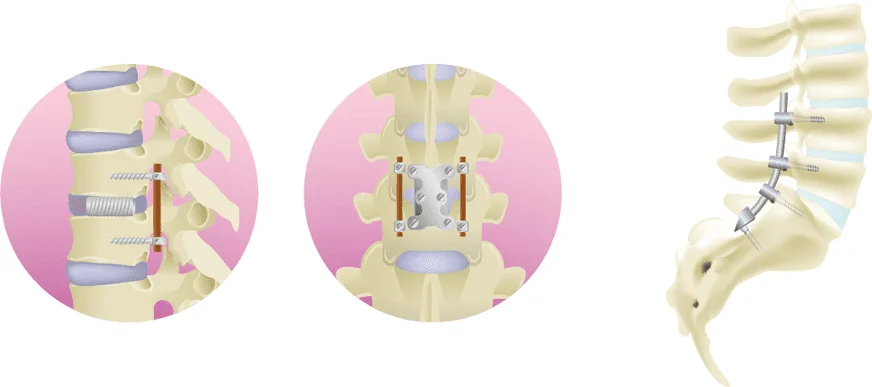
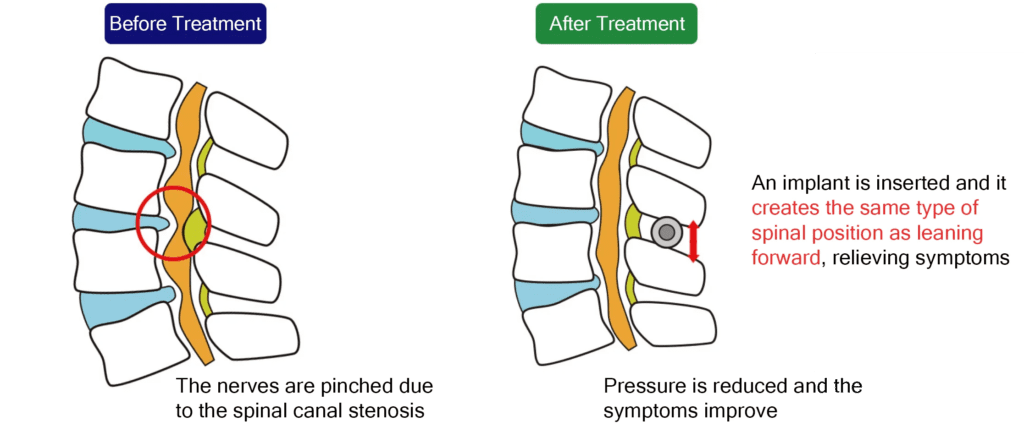
The Florence Method
The Florence method is a low-risk, minimally invasive treatment for spinal canal stenosis.
A spacer is inserted percutaneously under partial anesthesia and sedation to widen the narrowed spinal canal. It remains possible to remove the spacer if complications should arise after the treatment has been performed.
The Lobster spacer is inserted inside the vertebral body to stabilize it while preserving spinal rotation and flexion, widening the spinal canal, reducing disc protrusion, and reducing the thickening of the ligamentum flavum. Thus, the narrowed spinal canal is widened, and the pain is relieved.
It is recommended for patients whose condition has failed to improve with conservative treatment and who wish to avoid surgical procedures performed under general anesthesia, such as spinal fusion.
The Cellgel Method
Spinal canal stenosis occurs when a disc cracks, causing the central component to protrude and the protruding portion to cause the spinal canal to narrow. If the disc crack is not repaired, herniation can recur, and the spinal canal can become narrowed again.
The Cellgel method used at our clinics provides a fundamental treatment by injecting a drug that fills the cracks in the disc, which then forms a gel that replaces the cracks. It is characterized by the fact that the volume of the disc is not reduced, and the drug remains in the disc as a gel-like implant after treatment, thus preserving the disc.
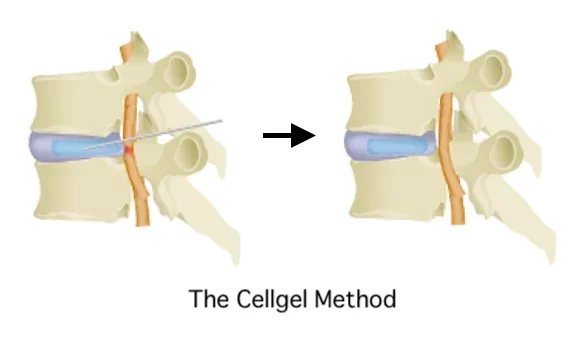
If you are suffering from spinal stenosis, please consider a consultation at our clinic.
Related Articles
The Different Symptoms of Spinal Canal Stenosis: If You Have Any of These, It’s a Red Flag!
How to Spend Time after Spinal Stenosis Surgery
Is it already too late! ? What should I do about spinal canal stenosis that has been left untreated?
What are the recommended rehabilitation methods for spinal canal stenosis that you can do yourself?