Have you visited multiple hospitals, but still suffer from a nagging pain that won’t go away?
Many people live with chronic pain or numbness for a number of years, only to be told that it is simply due to age or that it is in their head, and as a result must endure pain every day simply because imaging tests showed no clear cause for their symptoms.
The ILC Diagnosis used at our clinics does not attribute pain to just a single cause. Instead, it is a method that unravels a complex web of overlapping factors — such as disc degeneration, spinal curvature, and joint inflammation — to paint a thorough picture of your symptoms.
These factors do not exist in isolation. Rather, they are related and influence one another.
That is why treating only one finding often fails to improve symptoms — because other contributing factors remain untreated.
The ILC Diagnosis evaluates these elements comprehensively to clarify the full picture behind your symptoms.

The ILC Diagnosis reveals where pain truly originates, including causes that conventional imaging alone cannot detect.
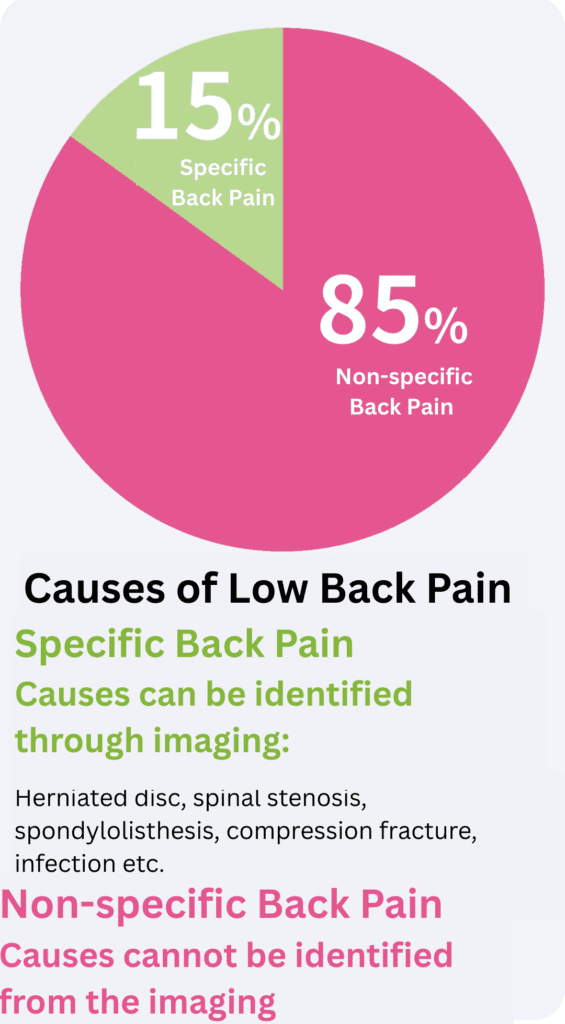
- Specific low back pain: 15%
→ The cause can be identified on imaging
→ Common examples:- Lumbar disc herniation
- Lumbar spinal canal stenosis
- Spondylolisthesis
- Compression fractures
- Infection
- Non-specific low back pain: 85%
→ No clear cause identifiable on MRI or X-ray
Source: Ministry of Health, Labor and Welfare (Japan): https://www.mhlw.go.jp/new-info/kobetu/roudou/gyousei/anzen/dl/1911-1_2d_0001.pdf (article in Japanese)
Low back pain is categorized into non-specific low back pain (85%), which is difficult to distinguish using imaging tests like MRI, and specific low back pain (15%), where the cause is usually more clearcut, like with disc herniation or spinal canal stenosis.
In addition to performing a standard MRI diagnosis, the ILC diagnosis analyzes these types of low back pain from multiple angles.
For specific low back pain (15%), imaging tests like MRI excel at identifying structural abnormalities in nerves or bones, such as disc herniation or spinal stenosis.
However, a significant portion of cases involve non-specific low back pain (85%), in which clear abnormalities cannot be found on MRI images.
The ILC diagnosis involves carefully reviewing symptoms like back pain, numbness, and walking difficulties, delving deeply into each patient’s lifestyle background.
By combining this information with the latest findings, we can uncover the causes of back pain that are invisible to imaging alone.
The Multiple Elements Contributing to Low Back Pain
While low back pain is often categorized as specific or non-specific, in real-life patients these elements almost always overlap.
While we primarily base our diagnostic on MRI images, which help identify the structural issues (the specific back pain), we also dig deep into the remaining 85% by listening to your life history and analyzing factors like muscle tension, blood flow, and nerve sensitivity (the non-specific back pain), which do not show up on scans and end up overlapping with one another, thus amplifying the pain.
By doing this, ILC diagnosis is able to evaluate and isolate each of these overlaps individually.
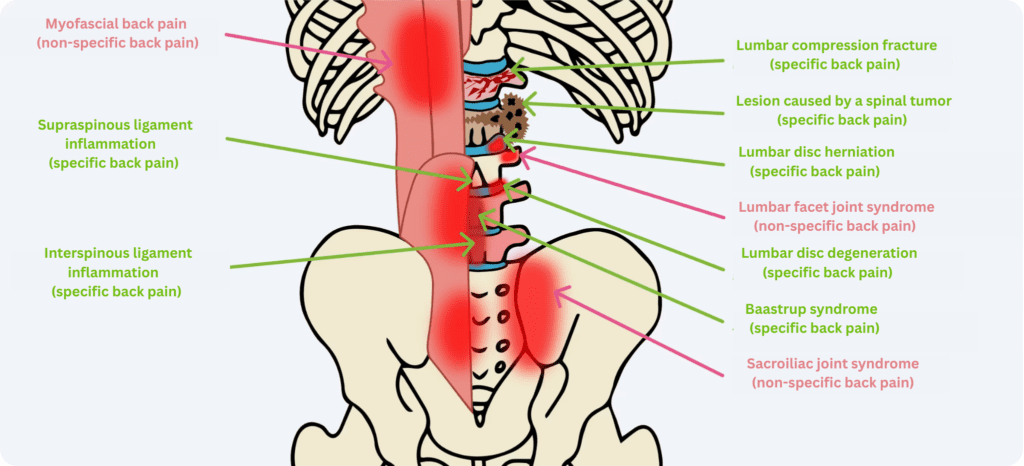
Specific Low Back Pain
 MRI System
MRI System
A device that captures cross-sectional images of the body without radiation exposure (to the difference of X-ray or CT scans).
 Conventional X-ray Imaging System
Conventional X-ray Imaging System
Used primarily to evaluate bone alignment and structural changes of the patient from the neck to the lumbar spine.
 Fluoroscopy System (Angiography)
Fluoroscopy System (Angiography)
Allows real-time visualization of the inside of the patient’s body on a monitor during the procedure, enabling precise and safe treatment.
Structural abnormalities such as disc herniation, bone deformity, or inflammation can be detected through MRI, X-ray, and physical examination.
MRI is extremely useful for identifying the causes of low back pain, with different sequences each highlighting various types of information — much like camera filters.
We will explain below the three main MRI imaging methods: “T1-weighted MRI,” “T2-weighted MRI,” and “STIR MRI.”
Each of these imaging techniques has their own merit, and physicians comprehensively analyze these images to zoom in on the true cause of pain.
T1-Weighted MRI: Used for Viewing the Structure of the Body
Fat appears white, and the boundaries of muscles and organs are clearly defined, making it ideal for checking on the shape of the brain, internal organs, and bone structure. It acts a bit like a city map: just as you can see the shape of the buildings and the layout of the roads on it, it also helps identify spatial relationships and structural issues within the body, and shows the clear boundaries of muscles and organs, helping identify bone irregularities or tumors.

T2-Weighted MRI: Used for Viewing the Anomalies of the Body
This technique excels at highlighting the water contents and inflammation caused by disease or abnormalities. Many conditions such as hernias, tumors, or strokes usually involve inflammation, which also increases the water content. Areas appearing bright white on T2 images likely indicate an unusual condition of some kind. Think of it as an X-ray highlighting the out of the ordinary in your body. In the same way that X-rays show fractures as white, T2 images will display inflammation as white. If, for instance, the area around the lumbar nerve is glowing white, indicating inflammation, it will provide important clues to help identify the cause of pain.

STIR MRI: Used for Detecting the Hidden Inflammation of the Bones and Muscles
Intentionally suppressing fat signals to make them appear completely black will highlight hidden inflammation or edemas as white spots. It is comparable to stars glowing in the darkness of the night sky. By eliminating the surrounding bright light (fat), faintly visible small lights (inflammation) become clearly discernible. This is highly effective for identifying pain causes difficult to detect with standard MRI, such as osteomyelitis, bone contusions, stress fractures, and edemas.
But can taking care of the structural abnormalities (specific factors) alone completely eliminate pain?
Besides the obvious irregularities visible on the images, there are always hidden functional irregularities (i.e. non-specific factors) that do not appear on the scan.
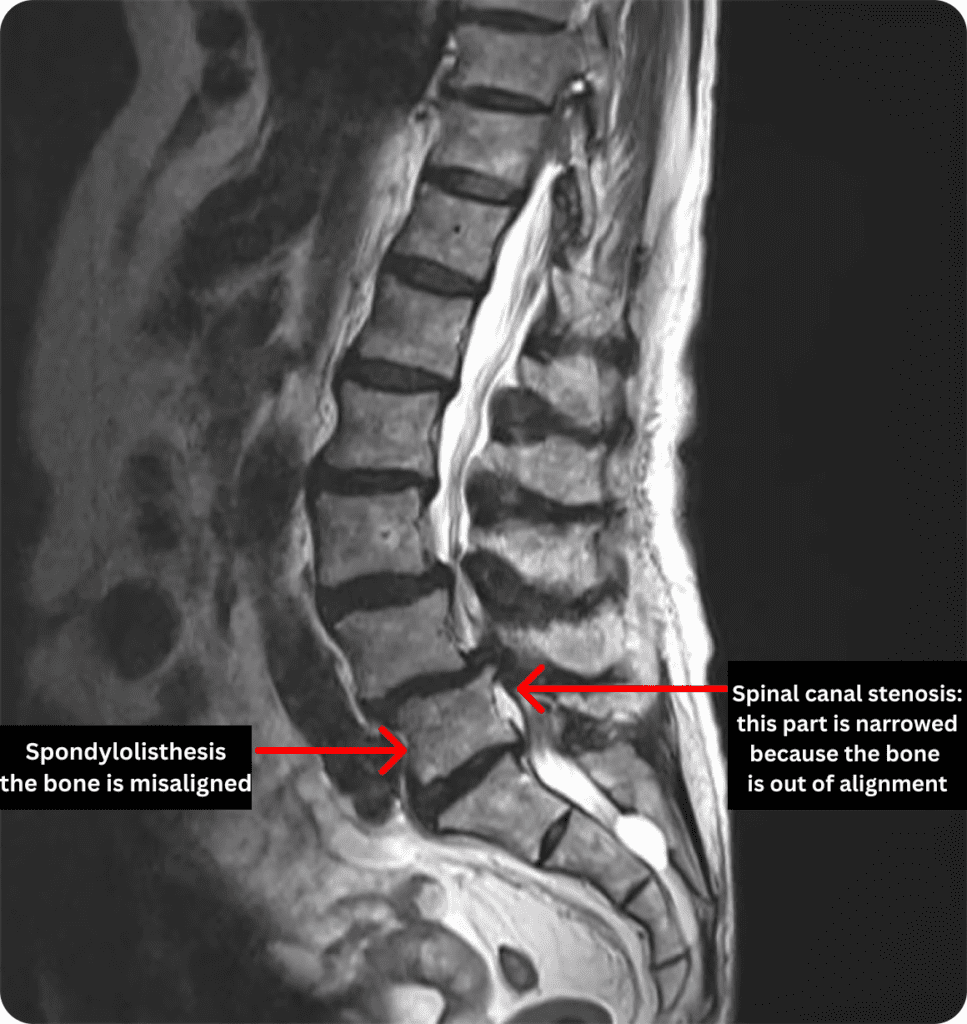
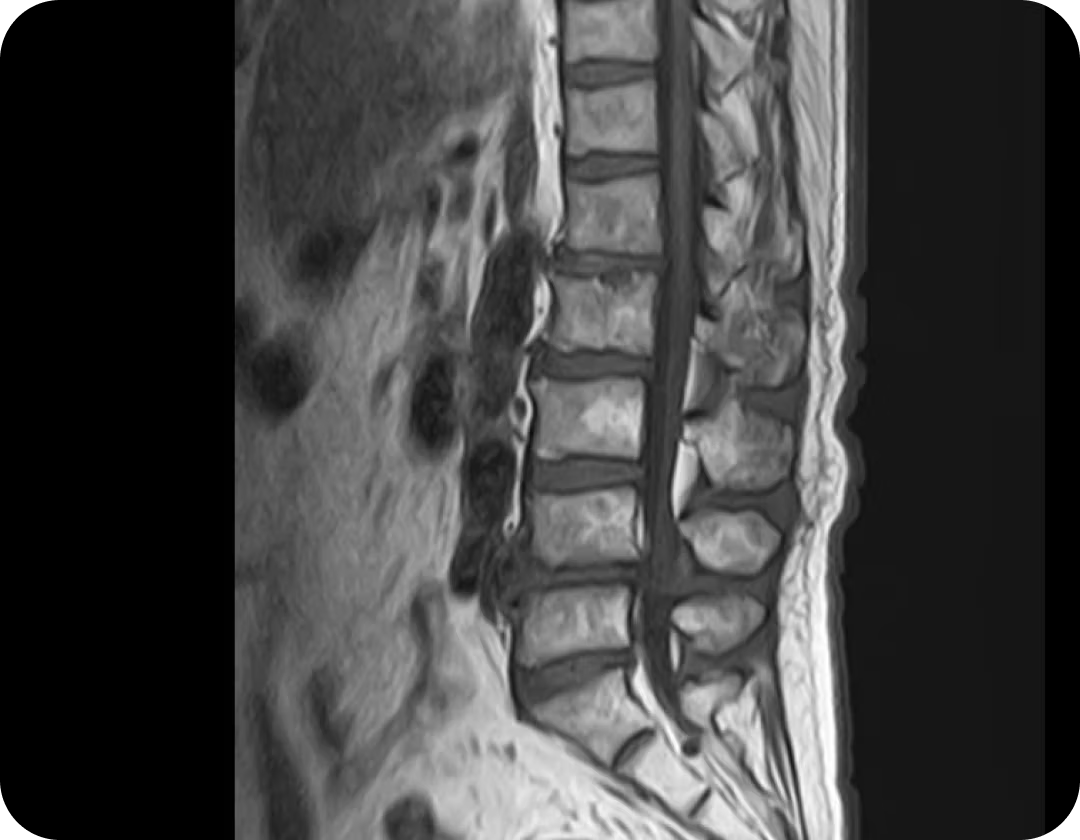
Spondylolisthesis + Spinal Canal Stenosis (example of combined conditions)
In the MRI image above, a negative chain reaction is occurring: the bone displacement (spondylolisthesis) is causing a narrowing of the nerve pathway (spinal stenosis).
So it’s not just about looking at the misalignment itself, but how it affects the nerves and surrounding inflammation. Unraveling this complex interplay is the essence of the ILC diagnosis.
Even if you receive a clearcut diagnosis like spondylolisthesis or stenosis (i.e. a specific low back pain diagnosis), it doesn’t necessarily mean the cause of the symptoms lies solely there.
Years of structural deformation almost invariably lead to factors not visible on imaging (non-specific factors) such as adjacent muscle stiffness, poor blood flow, and even nerve hypersensitivity.
The ILC diagnosis simultaneously assesses not only the imaging-visible diagnosis (specific factors) but also the accompanying body stress signals (non-specific factors). This is precisely why it is able to pinpoint the true nature of pain that hasn’t been resolved at other facilities.
Non-Specific Back Pain
Approximately 85% of low back pain is classified as non-specific—functional pain with no clear abnormality visible on MRI or X-ray.
Pain from functional abnormalities where no clear irregularity is found on MRI or X-ray is called non-specific back pain. Identifying such pain requires a multiple diagnostic approach to determine if the pain signals originate from the body or the brain.
Signals Originating from the Body
These refer to issues rooted in physical tissues or structures, which are difficult to detect with traditional imaging:
- Micro-inflammation/Damage to the Nerves: this occurs when nerves are slightly compressed or inflamed as a result from accidents or repetitive motions.
While MRI can show the nerve’s structure, it may not fully capture its proper function or subtle inflammation patterns. - Muscle Dysfunction: this is a condition where muscles do not function correctly, becoming excessively tense during specific movements or conversely losing strength.
This can place strain on joints and end up causing pain. - Fascial Adhesion: when the fascia covering the muscles stiffens and loses its ability to slide smoothly, it places limits on movement and lead to pain and stiffness.
These issues are often missed by standard MRI or X-ray imaging. The ILC diagnosis combines ultrasound imaging and a nerve conduction scan to identify such subtle problems and pinpoint the root cause of pain.
Signal Originating from the Brain
For pain previously deemed unexplained by conventional tests, we investigate in what way chronic stress, anxiety, and past traumatic experiences heighten pain perception.
- Comparison with the Physical Test Results
When signals from the brain arise, chronic stress, anxiety, or past traumatic experiences can cause the brain’s pain-processing areas to become hypersensitive.
As a result, even after physical issues are resolved, the brain may continue to send pain signals on its own. This can make even minor stimuli feel intensely painful, or pain to be felt in situations that should not normally cause discomfort.
The ILC diagnosis pinpoint these brain signals by first confirming, through a MRI examination, that there are no obvious physical causes. Detailed interviews and psychological assessments are then conducted. This allows for a comprehensive evaluation of whether the pain originates from physical causes or from excessive brain activity.
- In-depth medical questionnaire and Psychological Assessment
A detailed medical questionnaire is performed, covering when the pain began, at what times it intensifies, and any potential links to emotional stress or past trauma.
The timing of the increased pain may be associated not only with physical movements but also with mental stress, anxiety, or specific situations.
It is scientifically proven that anxiety, depression, and fear (including fear avoidance behaviors) can aggravate pain.
Using questionnaires that evaluate these psychological states, we determine the extent to which psychological factors may contribute to the pain.
- Neurological Function evaluation
We also verify whether peripheral nerves are functioning correctly and check on the presence and extent of nerve damage.
If pain persists despite the absence of issues during this examination, it generally means that the cause may lie in the functions of the central nervous system (i.e. the brain).
We then comprehensively analyze the root cause of pain by utilizing findings from cutting-edge research, such as fMRI, in addition to conventional imaging diagnostics like MRI.
Looking Beyond the Diagnosis — The ILC Approach: A Message to All the Patients Who Have Received a Medical Diagnosis Before
 Knowledge Is Key
Knowledge Is Key
What appears on your MRI images can be compared to a tree’s growth rings, but inside your body — evidence of the long years of hard work devoted to your loved ones and your job.
So, instead of denying the results of your imaging tests, let’s start by first embracing them.
Hearing unfamiliar, complex names such as “spinal stenosis,” “spondylolisthesis” thrown around by the doctor can sometimes feel unsettling, but these are merely a reflection of the natural changes occuring in your body, much like wrinkles appearing on an aging face.
The misalignments and narrowing in your bones are your lower back’s ‘medal of honor’ for supporting your family and the accumulated years of walking.
The pathology represents a testimony of how hard you’ve worked until now.
So first things first, please give your body, which has worked so hard on your behalf, some long-deserved thanks and appreciation.
Being able of putting a name on your specific medical condition at last does not mean that your body has finally given way and is not good anymore.
What matters more than what is on the MRI is how you can cope and make the best of this body in order to live comfortably from now on.
 Thinking is Paramount
Thinking is Paramount
The Venerable House Metaphor
Think of your body as a venerable house that is beginning to show its age.
A house’s structural age does not necessarily determine how comfortable it is to live in. The wear and tear of your home and its livability are two separate matters.
Let me explain why pain can vary, even with visible abnormalities on an MRI, using the analogy of the old house.
The Exterior and The Roof: What is Visible on the Images (the Diagnosis of the Pathology) (Specific)
Loose roof tiles (spondylolisthesis) or misaligned pillars (canal stenosis)
In a 50 or 60-year-old house, these are natural occurrences and do not necessarily make the house unfit for living.
Some tiles have shifted out of place (i.e. spondylolisthesis), and one pillar is misaligned (canal stenosis).
These are perfectly normal occurences in a 50 or 60-year-old house. These factors alone won’t make the house unhabitable, don’t you think?
The Interior of The House (the True Cause of Pain) (Non-specific)
Poor ventilation (blood flow): the blood tends to stagnate around the nerves.
Room chilliness (stiff muscles): muscles get stiff and cold.
The anxiety of the resident (psychological factors): the fear of the house collapsing one of those days contributes to heightened sensitivity to pain.
Although straightening the pillars (i.e. the pathology) would involve a full-scale renovation, the simple act of improving the ventilation and warming up the rooms (adjusting blood flow and muscle flexibility) can make a whole world of difference in terms of general comfort. The same applies to the lower back: even without changing the general structure of the bone (specific), adjusting blood flow and muscle flexibility (non-specific) can go a long way to make the pain surprisingly easier to manage.
 Performing Key Adjustments
Performing Key Adjustments
The Rusty Pipe Metaphor
Why does pain vary from day to day? Why does walking cause pain? Let’s explain using the analogy of the rusty pipes and water flow.
Spinal stenosis is a condition similar to a slightly rusty water pipe whose flow has narrowed as a result. However, if the water inside (i.e. the blood circulation) flows smoothly, there is no reason for it to clog.
However, when the body gets cold or remains still for too long, the water becomes thick and sludgy, making clogging (i.e. pain) more likely to occur.
Even if altering the pipe’s thickness (stenosis) is not an option, you can still choose to improve the water flow (i.e. the blood circulation) on your side starting today.
keep warm
Try soaking at length in a warm bath. This alone will resolve the hidden cause that is not visible on the imaging: the insufficient blood flow (non-specific factor).
keep swaying
By not strengthening, but loosening the muscles. Simply sway your hips like a swimming goldfish during walks or light exercises to remove the “rust” from your muscles (exercise therapy).
Take the sunlight in
Staying indoors due to the pain is actually the worst choice possible in that instance. Just walking a bit around your neighborhood to soak up sunlight shifts your mood away from the small stress weighing on your mind, thus quietening the brain’s pain sensors (psychological stress).
 Treating Your Self “As a Whole”, not Just That Single Spot of Pain
Treating Your Self “As a Whole”, not Just That Single Spot of Pain
Why has your back pain failed to heal so far?
One reason might be because so far you’ve only tackled that single abnormality visible on your MRI scan.
Lower back pain arises from a complex interplay between bone deformation, nerve inflammation, muscle tension, and mental anxiety.
Treating just one of these causes, while leaving the others untreated, will fail to fully improve your symptoms durably.
The ILC Diagnosis used at our clinic meticulously unravels the complex chain of pain — not only diagnosing conditions visible on MRI scans like bone deformity or nerve inflammation (specific low back pain), but also addressing the accompanying muscle tension and mental anxiety (non-specific low back pain) that are the body’s cries for help.
We help the patient reclaim a pleasant life free of pain by looking at each patient as a whole, not just what is visible on the imaging.
So, let’s find the exit strategy to your back pain together today.