March 14, 2025
Disc herniation is a common spine disorder. Once a disc herniates, symptoms such as pain and numbness can occur, and the more advanced the herniation, the more it will interfere with daily life.
Rehabilitation after surgery or any other treatments for disc herniation is also important, that is why in this article we will discuss what type of rehabilitation is necessary after receiving treatment for disc herniation.
What is disc herniation?
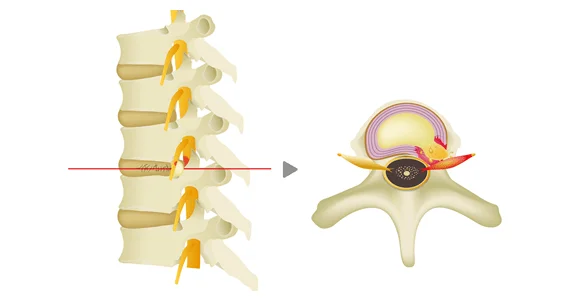
Intervertebral discs are located between vertebrae. The disc is composed of a gelatinous nucleus pulposus in the center and a collagen-rich annulus fibrosus that surrounds the nucleus pulposus.
When the annulus fibrosus develops a crack and the nucleus pulposus protrudes outward as a result, the condition is referred to as disc herniation.
Treatment of disc herniation
Treatment for lumbar disc herniation can be broadly divided into conservative therapy (medication, exercise therapy, etc.) and surgery.
Conservative therapy
Once disc herniation has been diagnosed, conservative therapy is usually the first step in most cases.
Medication include non-steroidal anti-inflammatory analgesics, muscle relaxants, opioid analgesics, and neuroleptics to reduce inflammation and pain. In addition, stretching and other rehabilitative measures may be used to improve back pain.
Nerve blocks may be used if the pain is severe or there is no improvement with medication.
Surgery
Surgery for lumbar disc herniation varies depending on the medical facilities.
Surgery methods vary, but in recent years, endoscopic surgery has become more common. An incision is made in the back under general anesthesia, a cylinder and endoscope are inserted, and the herniated area is removed while the location of the hernia can be seen through the endoscope in real time.
If the herniation has progressed to the point where spinal canal stenosis or spinal instability is present, spinal fusion surgery may be performed, in which not only the herniated area but also the disc in question is removed and replaced with an artificial one to secure the vertebrae in place.
Treatment of the intervertebral discs
Unlike the common surgical procedure which involves removal of the herniated area, disc therapy, which deals with the damaged disc, has become available in recent years. In contrast to conventional surgery, this treatment does not require hospitalization and can be performed as a one-day procedure.
・Percutaneous Ozone Disc Decompression (PODD)
PODD is indicated for mild herniation that does not require surgery and which does not respond to conventional conservative treatment.
A needle is inserted into the affected disc from the back under local anesthesia, and a mixture of ozone and oxygen gas is injected through the tip of the needle. Ozone oxidation reduces the volume of the herniated disc and relieves pressure on the nerves. It also has an anti-inflammatory effect on the affected area, thus minimizing the risk of side effects and complications.
・The Cellgel Method (repair of the intervertebral discs with a gel implant)
This is one of the advanced methods that have been researched and developed in recent years and this new treatment is backed by solid evidence.
This method is considered a curative treatment because it can effectively “repair the disc,” which is not possible with the other methods of treatment. It is characterized by the fact that the volume of the disc is not reduced and the drug remains in the disc as a gel-like implant after treatment, thus preserving the disc.
It is applicable not only to disc herniation, but also to a wide range of other conditions, and can be used for those who have had no pain relief after surgery or experienced a recurrence of pain, as well as for elderly patients over 80 years of age.
Why is post-treatment rehabilitation important?
Surgery and other procedures may remove nerve compression, but if muscle weakness and poor posture are not corrected:
・The risk of recurrence may increase.
・The back strain will not diminish, and chronic pain may persist.
・Muscle weakness and difficulty in movement may remain.
This is why rehabilitation is so important to reduce such potential adverse effects.
Rehabilitation will decrease the strain on the back and allow the patient to return to a more comfortable lifestyle.
Postoperative rehabilitation process and specific methods
Post-operative rehabilitation is a three-step process.
① Move as much as pain will allow immediately after treatment (1 to 2 weeks)
You should incorporate foot stomps and heel lifts in your daily routine, and perform them about 5 to 10 times at regular intervals. For example, do foot stomps and heel lifts while going to the toilet. Also, try doing draw-ins that can be done when you lying in bed, such as in the morning or at night.
・Heel Lift Exercise
Heel lift exercises help strengthen the calf muscles. Also considered as the secondary heart, the calf muscles are essential for standing and walking. This exercise is also recommended for people who tend to lose their footing frequently.
1. Spread your feet apart shoulder-width and put your hands on the wall to prevent from wobbling.
2. Lift your heels upward as if stepping on the floor with your toes.
At this time, you should feel strength surging in your calves.
*Note: Put your hands on the wall, but avoid putting weight on your hands.
The key is to repeat the exercise frequently, about 5 to 10 times a day!

・Draw-in
Draw-in is a core training exercise that strengthens the inner muscles through the movement of depressing and expanding the abdomen.
1. Lie on your back and bend your knees.
2. Inhale deeply and expand your abdomen.
3. Once your abdomen is fully inflated, slowly breathe out through your mouth and let your stomach contract.
* Hold the position for 5 seconds.
Repeat 5 to 10 times for 2 to 3 sets.
Feel the strength surge under your navel (in the tanden) and in your sides.

② Combine exercises to increase flexibility of the waist and spine with exercises to strengthen the core through stretching.
・Pelvic tilt exercise
This exercise is known to improve the flexibility of the lower back and spine. It also improves the movement of the pelvis and hip joints and reduces the strain on the lower back.
1. Sit on a chair so that the pelvis is perpendicular to the floor.
2. Move the top of the pelvis backward.
Repeat steps 1 to 2 for about 1 minute.
* Do it gradually at first, and for no longer than 3 minutes at the most. Relax and do not hold your breath.

・Bridge
This exercise strengthens the muscles of the back (trunk), buttocks, and backs of the thighs.
1. Lie on your back and bend your knees.
* Place your arms next to your body, with your feet, legs and knees spread apart by the width of one fist.
2. Push toward the floor with your head/shoulder blades so as to lift your hips and support your torso.
3. Hold the posture so that your shoulders are in a straight line from your shoulders to your knees for about 1-2 seconds, then slowly lower your back to the floor, starting with your back and then your buttocks.
Be careful not to hold your breath while performing this exercise.
Repeat10 times for 2 to 3 sets.

③ Full-scale exercise and improvement of everyday routine to be performed one month after treatment
Be aware of correct posture to reduce the strain on the lower back. Squatting and light strength training will strengthen the stability of the lower body.
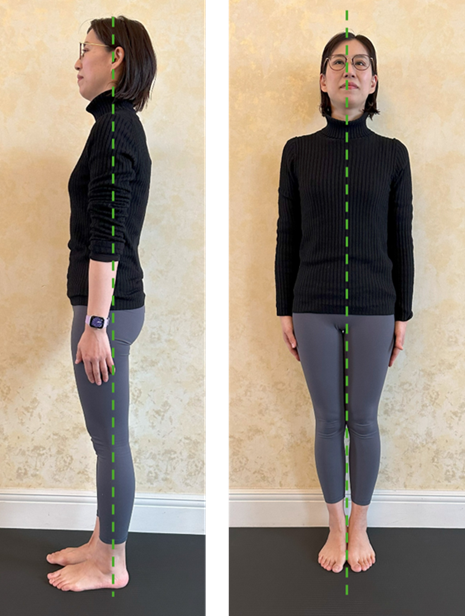
・Correct posture
Readjust your standing posture if you have difficulty standing.
(Posture as viewed from the side)
The correct posture is when the line connecting the outer ankle, greater trochanter, shoulder, and ear forms a single line.
Correct your hunched back or slouching posture as it puts strain on the lower back and shoulders and can cause pain.
(Posture as viewed from the front)
The posture should be symmetrical around the line connecting the nose, sternum, navel, legs and feet.
If either shoulder is elevated, lower the elevated shoulder to make it symmetrical.
Points of caution during the rehabilitation exercises
Do not do hard exercises right away, and do not push yourself too hard.
If you overdo it, it will have the opposite effect, so do not be too impatient and proceed step by step.
Stop exercising as soon as you feel pain. It is not a good idea to say, “I’m in a little pain, but I’ll force myself some more…”. Do not overdo it and consult your doctor or physical therapist immediately.
Be aware of proper form when exercising. Incorrect posture and movements can cause strain on the lower back. It is also a good idea to have them checked by a rehabilitation specialist.
If you have ever been diagnosed with disc herniation or are suffering from back pain, please consider a consultation at our clinic.
Related Articles
Properly Understand Herniated Discs and Get Proper Treatment
What is Lumbar Disc Herniation? Causes of Pain and Symptoms
Various Treatments for Lumbar Disc Herniation: Respective Differences and Results of Each Method
Is Disc Herniation for Teens and Young Adults on The Rise?
Symptoms and Treatments of Disc Herniation: When Early Detection is Key
Professional Athletes Who Have Battled With Disc Herniation in the Past – vol.1 – Kensuke Kondo
Professional Athletes Who Have Battled With Disc Herniation in the Past – vol.2 – Sani Brown